Madelung Deformity
Raymond Liu, M.D.
Tibial hemimelia (also known as tibial deficiency) is a condition in which a child is born with a tibia (shinbone) that is shorter than normal or missing altogether. This creates a difference in the length of the child’s legs. The condition is extremely rare, occurring in only about one out of every one million births. There are about four new cases in the United States each year.
Sometimes, tibial hemimelia runs in a family or is part of a medical condition. Most of the time, however, doctors are not able to determine exactly why the tibia is shorter.
Almost all children with tibial hemimelia will need surgery to help them stand, walk and play better. The type of surgery needed depends on several different factors, including how much of the tibia is present and the condition and stability of the child’s knee and ankle joints.
Anatomy
The lower leg is made up of two bones: the tibia and fibula. The tibia is the larger of the two bones. It supports most of your weight and is an important part of both the knee joint and ankle joint.
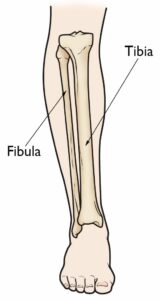
Tibial hemimelia is a partial or total absence of the tibia, which is the larger bone in your lower leg.
Description
Tibial hemimelia is a congenital condition, which means that it is present at birth. In the mildest cases, there may be only minor shortening of the tibia. In the most severe cases, the tibia may be missing entirely. Tibial hemimelia usually affects only one leg but, in about one-third of cases, both legs have the condition. When one leg is affected, it is usually the right leg, although doctors do not know why this is.

A baby boy with tibial hemimelia affecting both legs.
Reproduced from Krajbich IJ: Lower limb deficiencies and amputations. J Am Acad Orthop Surgeons 1998; 6:358-367.
Types of Tibial Hemimelia
Doctors usually divide tibial hemimelia into four different types, based on how much of the tibia is missing. Knowing the specific type will help your doctor develop the best treatment plan possible for your child.
-
- Type I. In this type, the tibia is missing in its entirety. As a result, the child’s knee and ankle joints do not usually work.
- Type II. In this type, the lower half of the tibia is missing. The knee joint usually works somewhat normally, but the ankle joint does not work.
- Type III. In this type, the upper half of the tibia is missing. As a result, the knee joint does not usually work, but the ankle joint may work somewhat normally. This type of tibial hemimelia is extremely rare.
- Type IV. In this type, the child has a shortened tibia and the lower ends of the tibia and fibula bones, near the ankle joint, are separated from each other. This causes the ankle joint to be very abnormal.
Other Medical Problems
Many children with tibial hemimelia are born with other problems involving their feet and legs, such as:
-
- A shortened femur (thighbone)
- A bifid femur (the bottom end of the thighbone is split into two)
- An absent extensor mechanism (the muscles, ligaments, and other structures that help the knee to straighten are missing)
- Clubfoot (the foot is turned inward)
- Absent toes or too many toes
Some children with tibial hemimelia may also have conditions that affect the arms.
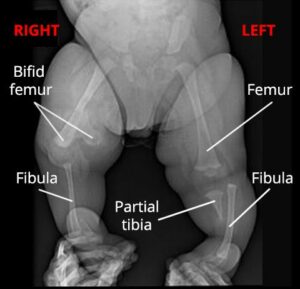
X-ray shows a healthy 7-month-old boy with tibial hemimelia of both legs. On the right side, the bottom end of his femur is split into two (bifid femur) and his tibia is missing. On the left side, his femur appears relatively normal, but the bottom half of his tibia is missing.
Cause
Most of the time, doctors do not know exactly why a baby is born with tibial hemimelia. Occasionally, however, the condition can be passed on through a family.
Sometimes, tibial hemimelia is associated with a medical condition or syndrome that affects multiple parts of the body, such as Werner’s syndrome, Langer-Giedion syndrome, and CHARGE syndrome.
Doctor Examination
Severe cases of tibial hemimelia are usually detected before the baby is born, during a prenatal ultrasound. Milder cases may not be recognized until after birth when the parents notice a difference in leg length as their child grows.
Medical History and Physical Examination
Since tibial hemimelia can sometimes be hereditary, your doctor will ask whether your family has any known medical syndromes or if there is a family history of short tibias.
During the exam, your doctor will carefully measure the lengths and widths of your child’s arms and legs. He or she will also move your child’s legs and feet in different ways to learn more about the knee and ankle joints. The exam will not be painful.
Tests
Tests will help your doctor confirm the diagnosis and guide your child’s treatment plan.
X-rays. X-rays provide images of dense structures, such as bone. Your doctor may order x-rays of your child from his or her hips down to the feet to determine which bones are present and which are missing. X-rays will also help your doctor estimate the difference in the length of your child’s legs.
X-rays can be performed as soon as your child is born. Although not all of the bone can be seen during infancy, a great deal can still be learned about the shortened tibia during this first set of x-rays.
Magnetic resonance imaging (MRI) scans. Your doctor may order an MRI to learn more about your child’s knee and ankle joints. The condition of these joints is very important in making treatment recommendations.
Genetic testing. If your child’s tibial hemimelia is caused by a medical condition or syndrome, your doctor may recommend an evaluation by a genetic specialist.
Treatment
The goals of treatment are for the child’s leg to work as well as possible, be pain free, and be as close as possible in length to the leg on the other side by the time he or she is fully grown. Treatment for tibial hemimelia involves a team of medical specialists. The team may include an orthopaedic surgeon, a pediatrician, physical and occupational therapists, an orthotist, and a prosthetist.
Your child’s treatment plan will depend on many different factors, including:
-
- How much of the tibia is missing
- How well the knee and ankle joints work
- The difference in the length of the legs
- Your child’s overall health
- Your family’s preference for a certain procedure
Nonsurgical Treatment
Almost all children with tibial hemimelia will eventually need surgery to help them function better. In very mild cases, however, nonsurgical treatment can sometimes be an option until surgery is required.
Nonsurgical treatment may include:
-
- Wearing a shoe lift. If the child’s foot can fit in a shoe, a shoe lift can help to even out a smaller difference in leg length.
- Prosthetics. For a larger difference in leg length, an artificial device can be fitted over the shorter limb to allow the child’s foot to be flat on the floor. These types of “accommodative” prostheses become more difficult to make over time, however, and then some type of surgery is almost always necessary to allow the child to walk and stand better.
Surgical Treatment
The surgical treatments most often used for the management of tibial hemimelia are:
-
- Limb reconstruction and lengthening
- Limb amputation
Limb reconstruction and lengthening. For children with less severe cases of tibial hemimelia, limb reconstruction and lengthening may be a viable treatment option.
Reconstruction usually involves one or more surgeries to repair the bones, muscles, and joints that are affected by the hemimelia. This is followed by gradual lengthening of the leg using an external fixator.
The external fixator is worn until the lengthened bone is strong enough to support the patient safely.
Limb lengthening usually requires multiple operations over several years.
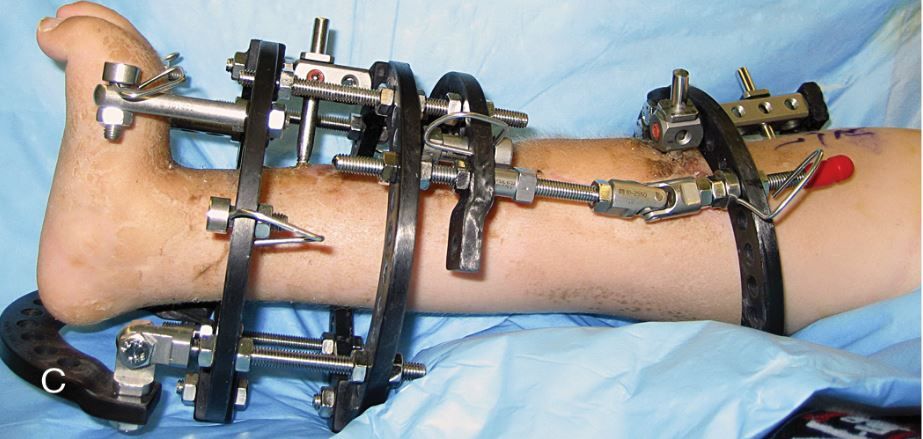
An external fixator may be used to gradually lengthen the shorter leg.
Reproduced from Hamby RC, McCarthy JJ (eds.): Management of Limb-Length Discrepancies. Rosemont, IL. American Academy of Orthopaedic Surgeons, 2011, p. 134.

Photo (left) and x-ray (center) show a boy with Type IV tibial hemimelia. He has a shortened tibia and the lower ends of his tibia and fibula bones are separated, making his ankle joint very unstable. (Right) After limb reconstruction and lengthening with an external fixator, he is able to place his foot flat on the floor. He will need a second (and possibly third) procedure in the future.
Reproduced from Hamby RC, McCarthy JJ (eds.): Management of Limb-Length Discrepancies. Rosemont, IL. American Academy of Orthopaedic Surgeons, 2011, p. 105.
Limb amputation. For many children with tibial hemimelia, limb reconstruction and lengthening may not produce the best outcome. For example, if the child has no functional ankle joint or is not able to actively straighten his or her knee (especially if the structures that enable the knee to straighten are missing) reconstruction and lengthening become more challenging.
In these situations, the best chance for the child to have an active life often involves amputation of the affected limb. After the limb is amputated, a prosthetist will fit the child for a prosthetic limb. The prosthetist will adjust the prosthesis or make a new one as the child grows.
The decision whether to opt for amputation is, understandably, a very difficult one for parents. Your orthopaedic surgeon and other medical specialists on your team will provide you and your family with support and education to help you determine which treatment option is best for your child.
Support
Living with—and having treatment for—tibial hemimelia can be both emotionally and physically challenging for a child and his or her family. Meeting other children with limb deficiencies and their families will provide reassurance that you are not alone and will be an invaluable source of information and support. You can find support and discussion groups for families of children with limb deficiencies online. In addition, your doctor may be able to put you in touch with families like yours so that you can meet and talk with them about their experiences.
Thanks to advances in prosthetics and limb reconstruction, most children with tibial hemimelia are eventually able to participate in almost any activity. It is important to help your child by being supportive and encouraging a positive self-image. If your child is struggling with either the emotional or physical aspects of treatment, be sure to share your concerns with your doctor.